How a simple blood test can reveal early signs of Parkinson’s
More than 1.1 million Americans live with the degenerative brain condition, which can trigger debilitating tremors and effect memory
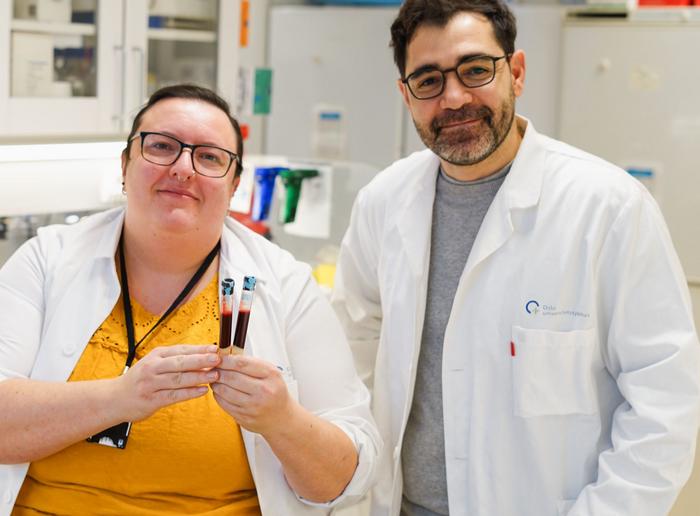
Newly-discovered markers in peoples’ blood can help identify the earliest signs of Parkinson’s disease years before symptoms start, Swedish researchers said Thursday.
While there is currently no cure for the degenerative brain condition that affects an estimated 1.1 million Americans and no test to diagnose the disease, early detection is crucial to administer treatments that can slow its progression.
A blood test for these markers could lead to earlier diagnoses, giving patients and doctors more time to respond.
“By the time the motor symptoms of Parkinson’s disease appear, 50 to 80 percent of the relevant brain cells are often already damaged or gone,” Danish Anwer, a doctoral student at Chalmers University of Technology, explained in a statement.
“The study is an important step towards facilitating early identification of the disease and counteracting its progression before it has gone this far,” Anwer added.
A crucial window
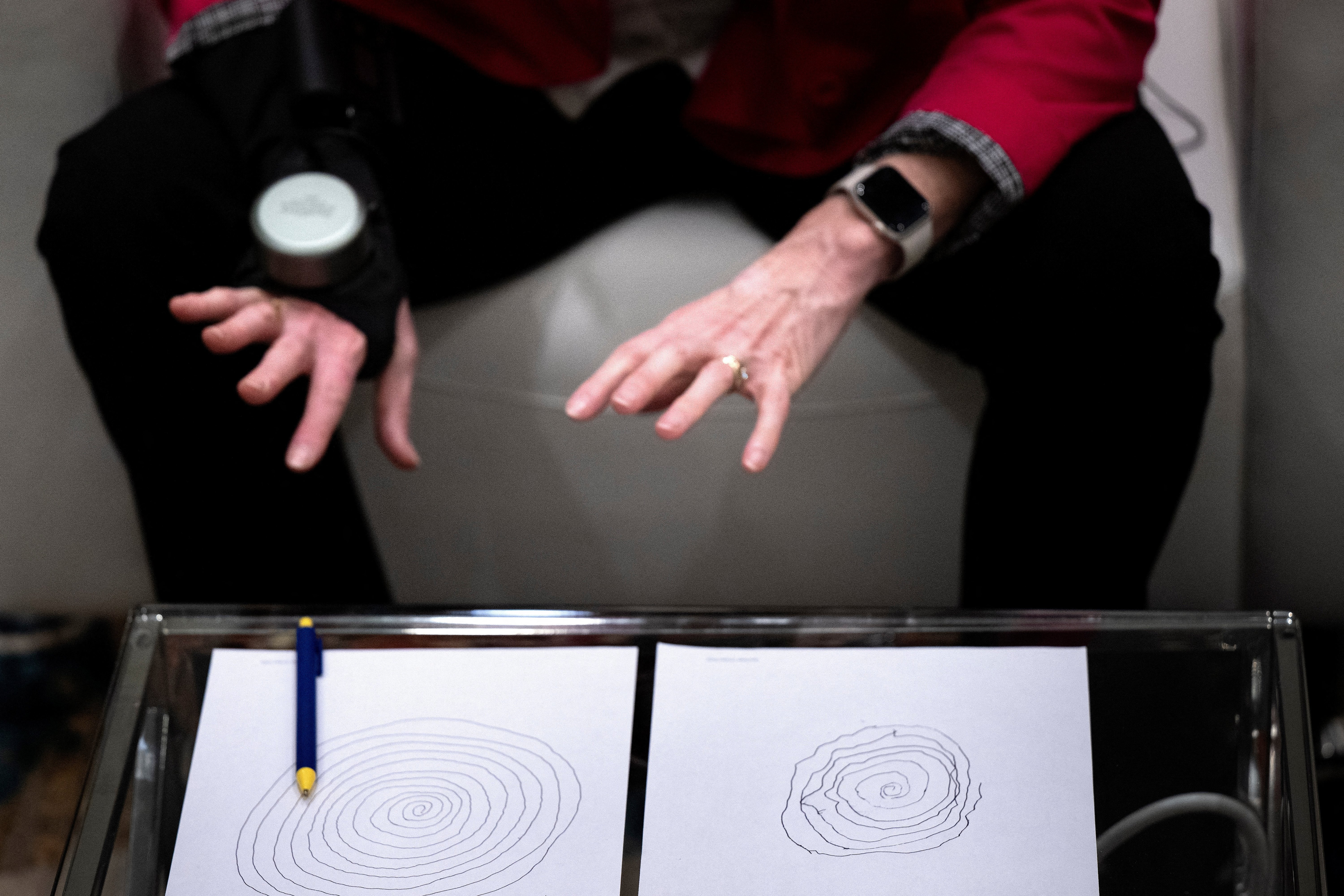
The biological processes that result in the disease leave traces in the blood, the university’s team found, but only for a short time, between the incubation of memory-impacting Parkinson’s and its symptoms.
To find these traces, the researchers focused on two processes long thought to be involved in the early phase of Parkinson’s - appearing up to 20 years before tremors and other motor symptoms are seen.
The first is the body’s ability to repair damage to DNA, and the second is cells’ response to stress. Both processes work to fix damage in our cells.
Using a type of AI known as machine learning, the researchers were able to identify a genetic pattern in people who weren’t healthy and didn’t yet have Parkinson’s symptoms.
This pattern indicated that both processes in the blood vessels were tied to the start of the disease.
“This means that we have found an important window of opportunity in which the disease can be detected before motor symptoms caused by nerve damage in the brain appear,” Annikka Polster, an assistant professor at the Department of Life Sciences, said.
Real world implications
Previous studies have identified other biological indicators of early Parkinson’s - looking in blood, brain fluid and even earwax.
A protein tied to cell loss in the brain called alpha-synuclein is the first widely used biomarker, according to the Parkinson’s Foundation.
But, tests for widespread screening to detect early Parkinson’s are not yet available and doctors have to rely on symptoms and medical history to make a diagnosis.
Motor symptoms typically start in people after they turn 50, but are sometimes seen in people as young as 20 years old, according to Mass General Brigham.
The Chalmers researchers say their findings could lead to such a test within just five years, as well as contribute to drug development.
“If we can study the mechanisms as they happen, it could provide important keys to understanding how they can be stopped and which drugs might be effective,” said Polster.
“This may involve new drugs, but also drug repurposing, where we can use drugs developed for diseases other than Parkinson’s because the same gene activities or mechanisms are active.”
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments
Bookmark popover
Removed from bookmarks