Why the US measles review matters as experts warn of wider risk
The re-evaluation is largely symbolic, contingent on whether a single measles chain has spread uninterrupted within the country
International health authorities are set to convene in April to determine if the U.S. has forfeited its measles-free designation, a year after an outbreak first emerged in West Texas.
Experts are concerned that the vaccine-preventable virus has re-established a foothold, potentially leading the U.S. to follow Canada in losing this significant public health achievement.
The re-evaluation is largely symbolic, contingent on whether a single measles chain has spread uninterrupted within the country for at least 12 months. Public health scientists are currently investigating potential links between the now-concluded Texas outbreak and active cases in Utah, Arizona and South Carolina.
However, medical professionals and researchers assert that the U.S. – and North America more broadly – confronts a significant measles challenge, irrespective of the upcoming decision.
“It is really a question of semantics,” said Dr. Jonathan Temte, a Wisconsin family physician who helped certify the U.S. was measles-free in 2000. “The bottom line is the conditions are sufficient to allow this many cases to occur. And that gets back to de-emphasizing a safe and effective vaccine.”
Last year, the Centers for Disease Control and Prevention confirmed 2,144 measles cases across 44 states — the most since 1991 — and nearly 50 separate outbreaks.
The problem has been years in the making, as fewer kids get routine vaccines due to parental waivers, health care access issues and rampant disinformation. More recently, Trump administration health officials have questioned and sown doubt about the established safety of vaccines at an unprecedented level while also defunding local efforts to improve vaccination rates.
“The most important thing that we can do is to make sure the people who aren’t vaccinated get vaccinated,” said Jennifer Nuzzo, director of Brown University’s Pandemic Center. “We have not issued a clear enough message about that.”
A Department of Health and Human Services spokesperson said Thursday that Health Secretary Robert F. Kennedy Jr. has consistently emphasized vaccines as the best way to prevent measles, adding that the CDC is responding to outbreaks and working to increase vaccination rates.
As of Thursday, the department said it doesn't have evidence that a single chain of measles has spread for a year.
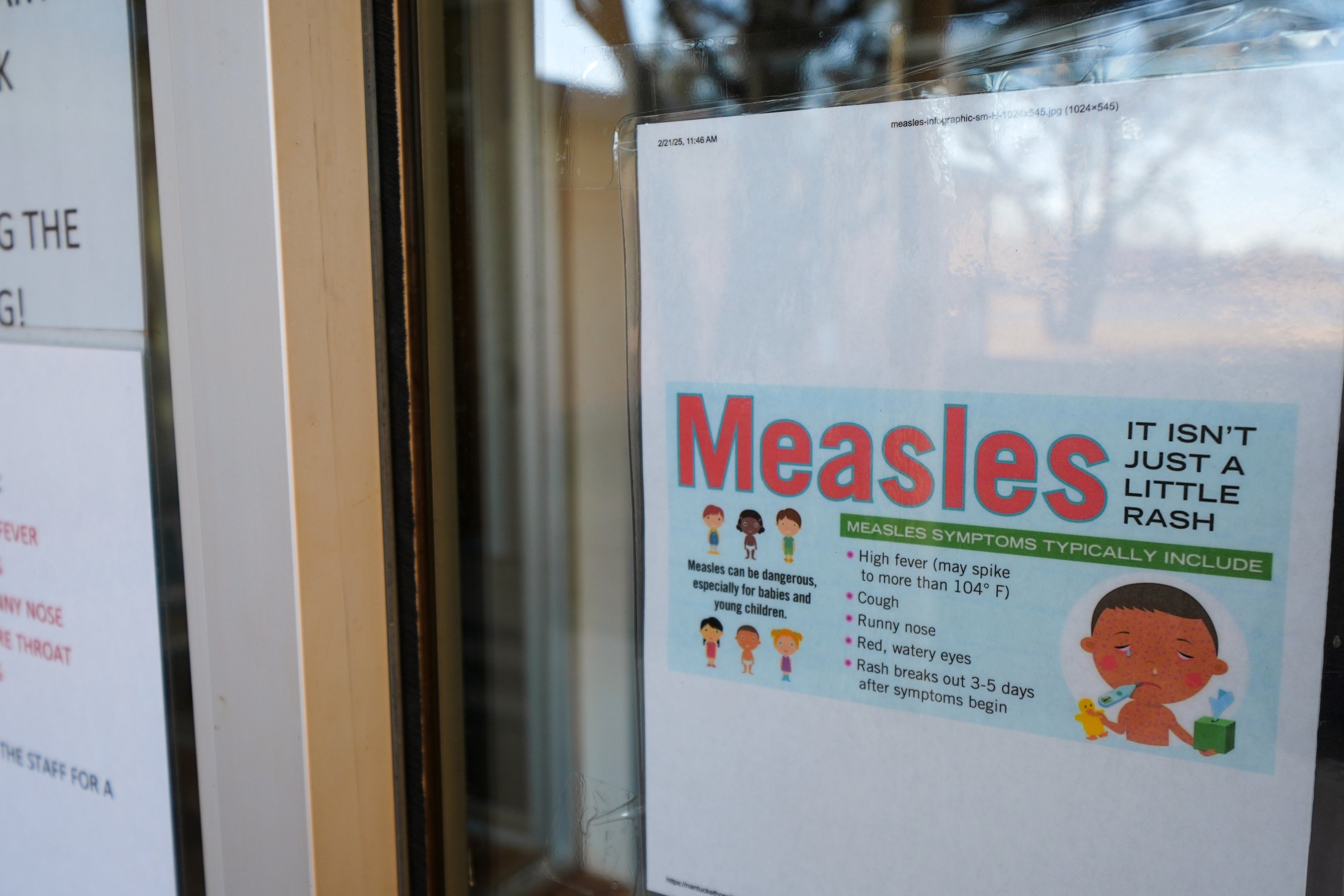
Measles finds the unvaccinated
There is little room for error in trying to stop measles. The virus is one of the most contagious, infecting 9 out of every 10 unvaccinated people exposed. Community-level protection takes a 95 percent vaccination rate. The current rate nationally is 92.5 percent, according to CDC data, but many communities fall far below that.
The patient in Texas’ first known case developed the telltale rash on Jan. 20, 2025, according to state health department data.
From there, the outbreak exploded. Officially, 762 people fell ill, most of them in rural Gaines County, and two children died. Many more got sick and were never diagnosed: 182 potential measles cases among children in Gaines County went unconfirmed in March 2025 alone, state health officials said, a possible undercount of 44% in that county.
Such data gaps are common, though, making it especially hard to track outbreaks. Many people living in communities where the virus is spreading face health care barriers and distrust the government.
Contact tracing so many cases is also expensive, said behavioral scientist Noel Brewer, who chairs the U.S. committee that will finalize the data for international health officials. Research shows a single measles case can cost public health departments tens of thousands of dollars.
CDC data on measles is still among the best worldwide, Brewer said, but “the U.S. has changed its investment in public health, so we’re less able to do the case tracking that we used to do.”
Genetic sequencing can fill some gaps.
But that's not always enough to say the outbreaks are connected. Genetically, the measles virus doesn't change as often as, say, flu.
“Within an outbreak, everybody is going to look the same,” said Justin Lessler, a University of North Carolina disease researcher.
The key question may then be how PAHO experts will navigate final data gaps, said Dr. Andrew Pavia, a Utah physician and longtime CDC consultant.
“My best guess is we will lose elimination status,” Pavia said. “The case for this not being continuous transmission is tenuous, and I think they are likely to err on the side of declaring it a loss of elimination status.”
Scientists have confirmed the same measles strain in Texas, New Mexico, Utah, Arizona, South Carolina, Canada, Mexico and several other North American countries, said Sebastian Oliel, a spokesperson for the Pan American Health Organization, which will make the final decision on U.S. measles elimination at an April 13 meeting.
Oliel said when there is a case of unknown origin in a country with ongoing local spread, “the most conservative approach is to consider the case part of the existing national transmission.”
Mexico also up for review
PAHO will review Mexico's measles-free status alongside the U.S., Oliel said. That country's largest outbreak has roots in Texas. It started when an 8-year-old boy from Chihuahua state got sick after visiting family in Seminole, Texas. Since last February, 6,000 people have gotten sick in Mexico, and 21 have died in Chihuahua state.
But under PAHO's definition of elimination, borders matter. If, for example, the chain of measles that started in the U.S. spread to Mexico and then returned to the U.S. anew, it would be considered a new chain, experts said. Still, many experts call that standard outdated.
What's clear is that measles found ample fertile ground in the U.S. in 2025, infiltrating schools and day cares, churches, hospital waiting rooms and a detention center. New Mexico logged 100 cases and one adult died. Kansas officials spent seven months trying to control an outbreak that sickened nearly 90 people across 10 counties. Ohio confirmed 40 cases. Montana, North Dakota and Wisconsin each had 36.
Now, more than 800 people have gotten sick across Utah, Arizona and South Carolina since late summer, with no end in sight.
“2025 was the year of measles,” Brewer said. “Will 2026 be the year of rising or falling measles cases? Does it get worse or does it get better? No one knows the answer.”
Bookmark popover
Removed from bookmarks