‘I earned more working at Amazon’ - Junior doctors explain why they are striking
Doctors tell the Independent why they decided to join the picket lines despite huge backlash
‘Fire fighting’ to keep patients stable, overspill into overcrowded hospital corridors and 12-hour waiting times are the bleak reality for NHS doctors across England.
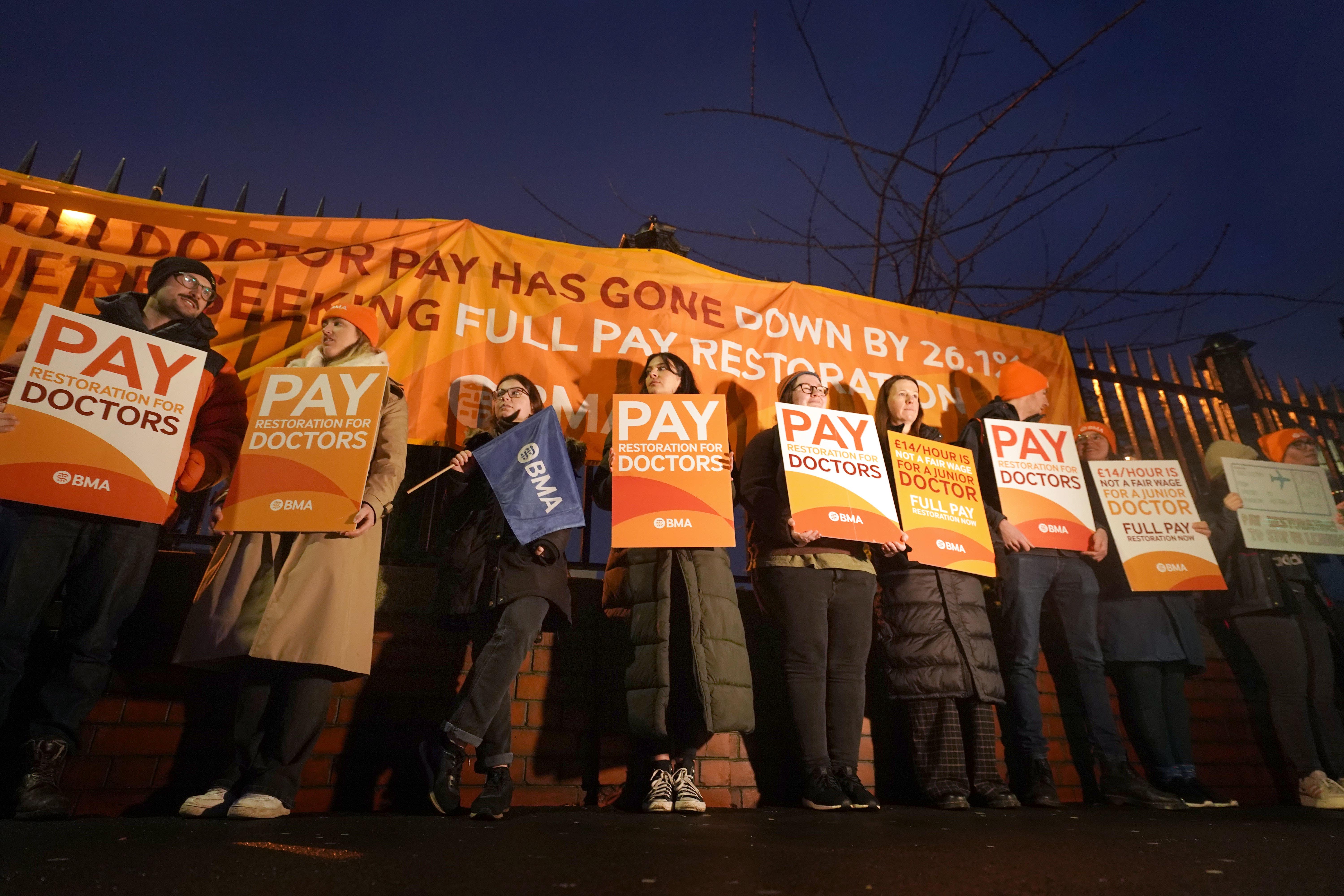
Junior doctors embarked on the longest strike in history last Wednesday to attempt to settle a longstanding pay dispute.
Campaigners for the British Medical Association (BMA) say their wages have not risen with inflation since 2008 - equating to a 26% loss in pay.
Medics all over the UK have stopped working to campaign for an hourly increase in pay for qualified doctors in their first year of work from £15.50 an hour to £21 an hour.
NHS doctors say dozens of their colleagues are leaving to work further afield in Canada, Australia, New Zealand and even closer to home in Ireland to establish better working conditions.
The government has not come to the table to discuss an offer with the medical union and the strike ended at 7am today.
Today, Health Secretary Victoria Atkins said she would sit down to negotiate with junior doctors if they enter talks with “reasonable expectations”.
‘I earned more working at Amazon’
Doctor Sumi Manirajan qualified from Warwick University Medical School in 2021 and currently works as an A&E doctor in North-West London.
She did an undergraduate degree in Clinical Science and then went to medical school in Warwick, she qualified in 2021 after amassing £100,000 of debt.

Last winter she worked as a general surgical senior house officer overseeing A&E patients in need of operations, she says she was paid £16 an hour.
In her first year of working, she says she was paid £13.80 an hour - less than when she worked delivering parcels for Amazon.
She said: “I worked for Amazon whilst I was a medical student and I got paid more than when I was a first-year doctor.
“I’m not going to say the Amazon job was perfect but if I was late to deliver a parcel to someone, it wasn’t a life or death situation.
“If I make a mistake as a doctor, my patient could die- that’s the level of risk we take on”
Doctors are put on rota to work 48 hours a week but often work a lot longer, explained Dr Manirajan.
She said: “The rota gaps and what I’m seeing because of that right now has the biggest effect on me.
“The NHS is 50,000 doctors short, we are working a rota that is severely understaffed.
“I have to see 20 patients in a 12-hour shift, it is categorically unsafe. I don’t have time in between patients to think, you’re just fire fighing, and stabilising people for as long as you can before the rest of the team comes in.”

Dr Manirajan described colleagues having breakdowns on shift and a collective feeling of overwhelming pressure as medics try the best they can to face the crisis - with many not coping and having to take time off sick- worsening the existing staff shortage.
As an A&E doctor, Dr Manirajan sees patients who are on the brink of life and death.
She said: “It’s manic in hospitals. I’ve seen patients outside in trollies in corridors waiting to be seen. One patient I saw recently made me think about the future of the NHS. I saw a lady come in with chest pain, which is a serious symptom.
“I became quite worried so asked her when the symptoms started. I found out the symptoms had started the day before, she had come in but had been waiting over 12 hours. The NHS is in a really sorry state.”
At the end of 2022, the Royal College of Emergency Medicine counted up to 500 unnecessary deaths due to crowding and excessive wait times.
The union says they are fighting to return to 2008 conditions when they say the NHS was the best healthcare system in the world, before the financial crisis.
On picket lines the South Australian Health Ministry routinely attempts to attract NHS doctors by the offer of a dream life in the sun with the promise of better working conditions and pay, Dr Manirajan revealed.

Dr Manirajan: “With every colleague that leaves, I think why haven’t I done that?
“Some of the best doctors I know left to go to Australia, every time it’s a shock but it’s never a surpirse.
“My friends going over serves as a reminder of how life could be.”
The young doctor’s dream is to become an obstetrician, but that would require at least seven more years of training- but there is not an easy linear route, she added.
Each specialty can require a different amount of years- and there is no guarantee doctors will pass the exams they have to fork out for and revise for around their hectic schedules.
Sometimes there is no opportunity to progress, she explained, in radiology there was only one training spot for every eight applicants, she added.
“I can understand the frustration of having an appointment and operation cancelled and I want to apologise to patients.
“In Scotland, not a single person missed about because the government met with them and accepted. Our government has a greater opportunity to do the same but they haven’t done that,” she added.
Mike Greenhalgh, 34, qualified in 2016 and works as a Trauma and Orthopaedic Surgery Registrar, in Manchester with an hourly rate of £24.
Dr Greenhalgh’s job involves seeing patients who need hip and knee replacements and assisting in their operations but he also deals with patients who come in through A&E.
He said: “I love my job, it’s a privilege to be a doctor. Pay has been cut by over a quarter, year upon year and enough is enough.
“We’ve reached a real point where if we don’t make a stand now, pay will continue to be chipped away at.”
Dr Greenhalgh explained the label ‘junior’ is an unsuitable term since it refers to all doctors who are not yet at consultant level, whether they have been working as a doctor for one day or 10 years.
Reminiscing on his early twenties, he says he often wonders whether he made the right decision when he could have opted for a well-paid graduate scheme.
To get through the years of training medics also have to cover expensive exams, to progress in his job and become a consultant he will have to pay £1904 for an exam.
The assessments he took last year cost £1625 and there are further costs of £260 a year for their portfolio, £140 for medical indemnity and a further £420 to the General Medical Council.
To complete his orthopaedic training, Dr Greenhalgh also has to pay £197 to the British Orthopaedic Association.
He added: “Patients face a 12 to 18 month waiting list and they’re in pain. This is another reason why doctors feel a need to take action.
“There are people who have waited months to see their GP and then even longer for a hospital appointment to come to the conclusion they need a replacement. We then have to tell someone who is visibly in pain that they have to wait a ridiculous amount of time to get one. Patients are understandably upset.”
“We wish we could do more, when we do our training and go into medicine it’s because we want to help people.
“I have dual citizenship with Ireland, people think we are spouting rhetoric with this, but I want to stay and work for the NHS it is one of the reasons I became a doctor.
“There are gaps everywhere, I show up to work when there are meant to be two doctors on call but one is unwell, and there is no one to take up the slack so I end up doing the work of two doctors and seeing people in A&E who have waited over 12 hours - they’re understandably very annoyed.”
Dr Greenhalgh explained doctors were the lowest-paid workers on wards on Christmas and New Years Day since they do not get paid holiday overtime like other NHS workers.
On Friday, Health Secretary Victoria Atkins told PA: “I’ve said throughout this that, please, to the junior doctors’ committee, the moment you call off the strikes I’ll get back around the table with you within 20 minutes.”
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments
Bookmark popover
Removed from bookmarks