Study finds school HPV vaccine also cuts cancer risk in unvaccinated women
Researchers have discovered new ‘herd effects’ of school-based vaccination programmes
A new study has found that high uptake of school-based immunisation against human papillomavirus (HPV) could also offer protection against the development of pre-cancerous cells in unvaccinated women.
Researchers suggest these “herd effects” support universal vaccination initiatives, particularly those that target teenagers.
HPV is common and is spread through skin contact, usually while having sex. While most strains are harmless, around 13 high-risk types are known to cause 99.7 per cent of cervical cancers.
In England, a vaccine to protect against HPV is offered to teenagers in Year 8, or aged 12 to 13.
The jab also protects against genital warts and head and neck cancers, such as those in the mouth or throat.

Experts in Sweden said that while previous research has shown the herd immunity effects of the vaccine on genital warts, its effects on pre-cancerous cervical cells in unvaccinated women were “less clear”.
The study, published in the Lancet Public Health, analysed Swedish national health registry data from 857,168 unvaccinated women born between 1985 and 2000.
They were split into four groups: opportunistic vaccination (1985-1988), or those who proactively sought the jab, subsidised programmes (1989-1992), catch-up programmes (1993-1998), and school-based vaccination (1999-2000).
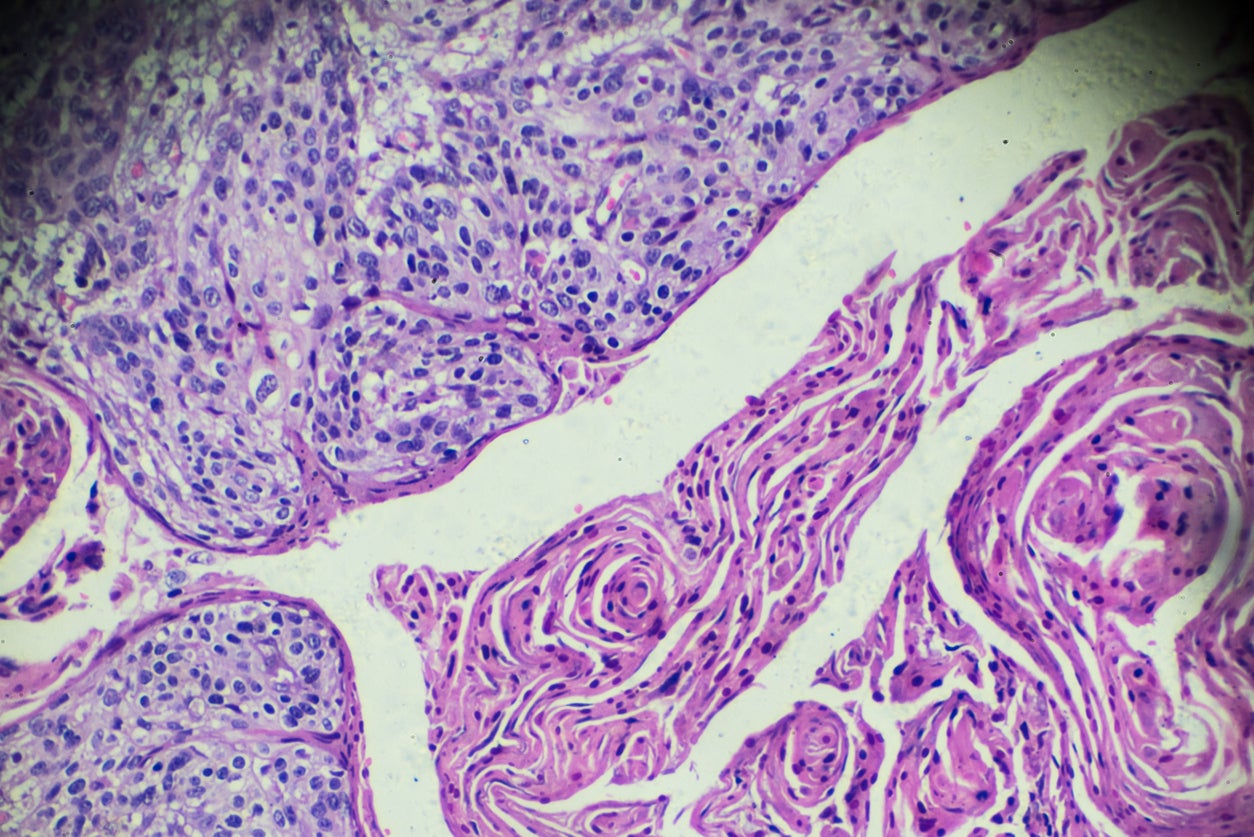
Researchers looked at the rates of high-grade cervical lesions – severely abnormal cells on the cervix caused by chronic HPV infection – which can develop into cancer if left untreated.
The team found “a substantially lower incidence” of these lesions among unvaccinated women in the group exposed to school-based vaccination compared to those in the opportunistic vaccination group.
Those born between 1999 and 2000 who did not have the jab in school had around half the risk of developing serious pre-cancerous changes compared with those born between 1985 and 1988.
“When combined with existing evidence, our findings support that high HPV vaccination coverage substantially reduces the incidence of high-grade cervical lesions in both the vaccinated population, through direct protection, and the unvaccinated population, through herd effects,” researchers said.
“These findings underscore the value of expanding school-based vaccination programmes as a cost-effective public health strategy to lower cervical cancer risk across entire populations.
“From a policy and implementation perspective, these results advocate for sustained efforts in universal vaccination initiatives, particularly those targeting school-aged populations, to maximise the benefits.”
The NHS is aiming to boost uptake of the HPV vaccine among girls to 90 per cent as part of plans to eliminate cervical cancer by 2040.
Data released in July shows that in the 2023/24 academic year, some 76.7 per cent of girls and 71.2 per cent of boys aged 14 to 15 were vaccinated against HPV by Year 10.
Uptake in Year 8 increased to 72.9 per cent among girls and 67.7 per cent among boys, from 71.3 per cent and 65.2 per cent respectively a year earlier.
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments
Bookmark popover
Removed from bookmarks